Introduction to Empagliflozin and Heart Failure
As a blogger, I've been following the recent developments in the medical field, and one topic that has caught my attention is the potential role of Empagliflozin in reducing hospitalizations due to heart failure. In this article, we will explore the basics of Empagliflozin, its mechanism of action, and its potential benefits for heart failure patients. So, let's dive in and learn more about this exciting new treatment option.
What is Empagliflozin?
Empagliflozin is a medication that belongs to a class of drugs called sodium-glucose cotransporter-2 (SGLT2) inhibitors. It is primarily used to treat type 2 diabetes by lowering blood sugar levels. It works by blocking the reabsorption of glucose in the kidneys, allowing excess glucose to be excreted through urine. This helps to maintain a healthy blood sugar level and reduces the risk of complications associated with diabetes.
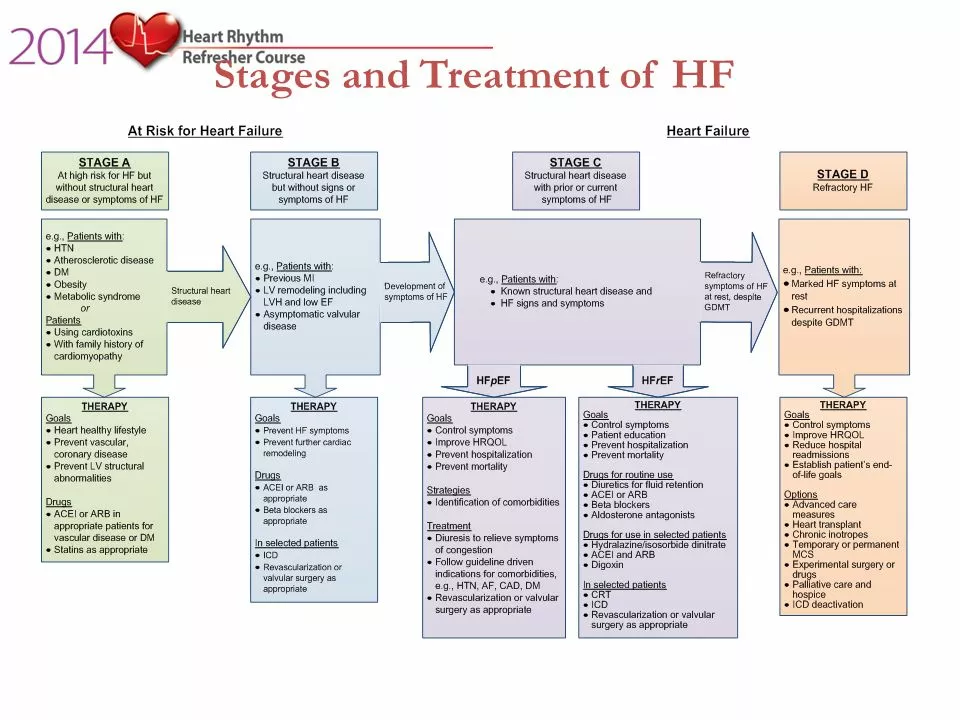
Heart Failure: A Growing Concern
Heart failure is a chronic condition in which the heart is unable to pump blood efficiently, leading to a reduced blood flow to the body's organs and tissues. This can result in symptoms such as fatigue, shortness of breath, and fluid retention. Heart failure is a common and serious health problem that affects millions of people worldwide. In fact, it is one of the leading causes of hospitalizations and death in the United States.
Empagliflozin's Role in Heart Failure Management
Recent studies have shown that Empagliflozin may have potential benefits for heart failure patients, even in those without type 2 diabetes. The medication has been found to improve heart function and reduce the risk of hospitalization due to heart failure. Its mechanism of action in heart failure is still not fully understood, but it is believed to be related to its effects on glucose metabolism, sodium reabsorption, and blood pressure regulation.
Reducing Hospitalizations: The EMPEROR-Reduced Trial
The EMPEROR-Reduced trial was a large, randomized, double-blind study that investigated the effects of Empagliflozin on heart failure patients with reduced ejection fraction (HFrEF), a condition where the heart's pumping ability is weakened. The study found that Empagliflozin significantly reduced the risk of hospitalization for heart failure and cardiovascular death in patients with HFrEF, regardless of their diabetes status.
Benefits for Patients with Preserved Ejection Fraction
Another important aspect of Empagliflozin's potential in heart failure management is its potential benefits for patients with preserved ejection fraction (HFpEF), a form of heart failure where the heart's pumping ability is relatively preserved but still not functioning optimally. Although the data on Empagliflozin's effects on HFpEF patients are still limited, preliminary results suggest that it may also have a positive impact on this group of patients, potentially reducing hospitalizations and improving their quality of life.
Empagliflozin's Safety and Tolerability
One of the main concerns when introducing a new medication into a treatment plan is its safety and tolerability. Empagliflozin has been shown to be generally well-tolerated by patients, with most side effects being mild and manageable. Some common side effects include urinary tract infections, genital infections, and increased urination. However, it is important to note that every patient is different, and it is essential to discuss the potential risks and benefits of any medication with a healthcare professional.
Empagliflozin as an Adjunct Therapy
It is important to note that Empagliflozin is not intended to replace current standard therapies for heart failure. Instead, it may be used as an adjunct therapy, which means that it is added to a patient's existing treatment plan to enhance its effectiveness. This approach allows healthcare professionals to tailor the treatment to each patient's individual needs and optimize their chances of success.
Moving Forward: Empagliflozin and the Future of Heart Failure Treatment
As we've seen, Empagliflozin holds promise as a potential treatment option for heart failure patients. Its ability to reduce hospitalizations and improve heart function may offer significant benefits to those struggling with this chronic and debilitating condition. As more research is conducted and we continue to learn about Empagliflozin's effects on heart failure patients, it is possible that this medication may become an essential part of the treatment arsenal for this challenging disease.



Listen up, the data on Empagliflozin isn’t just another fluff piece-it's a paradigm shift in cardiology. The EMPEROR‑Reduced trial demonstrated a statistically significant 25% drop in HF hospitalizations, which, for a field saturated with incremental tweaks, is a bold stride. This isn’t merely about glycemic control; it’s about modulating renal sodium handling and myocardial energetics in a way that traditional ACE inhibitors never touched. 🧐 Moreover, the drug’s safety profile holds up under scrutiny, with adverse events hovering around the low‑digit percentages seen in other SGLT2 studies. In short, we’re witnessing a therapeutic renaissance-brace yourselves for a new standard of care. 🚀