Medication Overuse Headache Risk Calculator
How often are you using headache medication?
Every year, millions of people reach for painkillers to quiet a headache-ibuprofen, Excedrin, triptans, even prescription opioids. It makes sense. Headaches hurt. But what if the very pills you’re taking to feel better are actually making your headaches worse? This isn’t rare. It’s called medication overuse headache (MOH), and it’s one of the most common reasons chronic headaches stick around when they shouldn’t.
What Exactly Is a Drug-Related Headache?
Medication overuse headache isn’t a new type of pain. It’s what happens when your body gets used to the drugs you take to treat headaches-migraines or tension-type headaches-and starts relying on them. Instead of stopping the pain, the medication begins to cause it. You end up with headaches more than 15 days a month, often daily, and the only way to break the cycle is to stop taking the medicine you thought was helping.
This isn’t about being addicted or abusing drugs. Most people who develop MOH are following their doctor’s advice, taking pills exactly as directed-until they start taking them too often. The problem isn’t the dose. It’s the frequency.
Which Medications Cause the Most Problems?
Not all pain relievers carry the same risk. Some are far more likely to trigger MOH than others.
- Triptans (like Imitrex, Zomig): Used for migraines. Overuse starts at 10 or more days per month.
- Opioids (oxycodone, tramadol, hydrocodone): Even occasional use-10 days a month-can trigger MOH. These are especially dangerous because they also carry addiction risks.
- Butalbital combinations (like Butapap, Lanorinal): These contain a barbiturate that’s highly addictive and triggers MOH at just 10 days per month.
- Combination analgesics (Excedrin, Midol): These mix caffeine, aspirin, and acetaminophen. Risk kicks in at 15 or more days per month.
- Simple NSAIDs (ibuprofen, naproxen): Lower risk, but still dangerous if you hit 15 days a month or more. The FDA says you shouldn’t take more than 1,200mg of ibuprofen or 660mg of naproxen sodium daily.
Here’s the catch: if you’re taking any of these on a regular basis-especially for more than three months-you might already be in the middle of MOH without realizing it.
How Do You Know It’s Not Just a Bad Headache?
MOH has a clear pattern:
- Your headaches happen on 15 or more days per month for at least three months.
- You’re regularly using one or more of the medications listed above.
- Your headaches feel different-often more constant, dull, and worse in the morning.
- You notice your painkillers work less and less over time.
- You start taking more pills just to get the same relief.
Many people think their headaches are getting worse because their migraine is progressing. But in over 85% of cases, it’s the medication itself that’s the problem. As Dr. Peter Goadsby from King’s College London put it, “MOH represents a failure of treatment strategy, not patient behavior.”
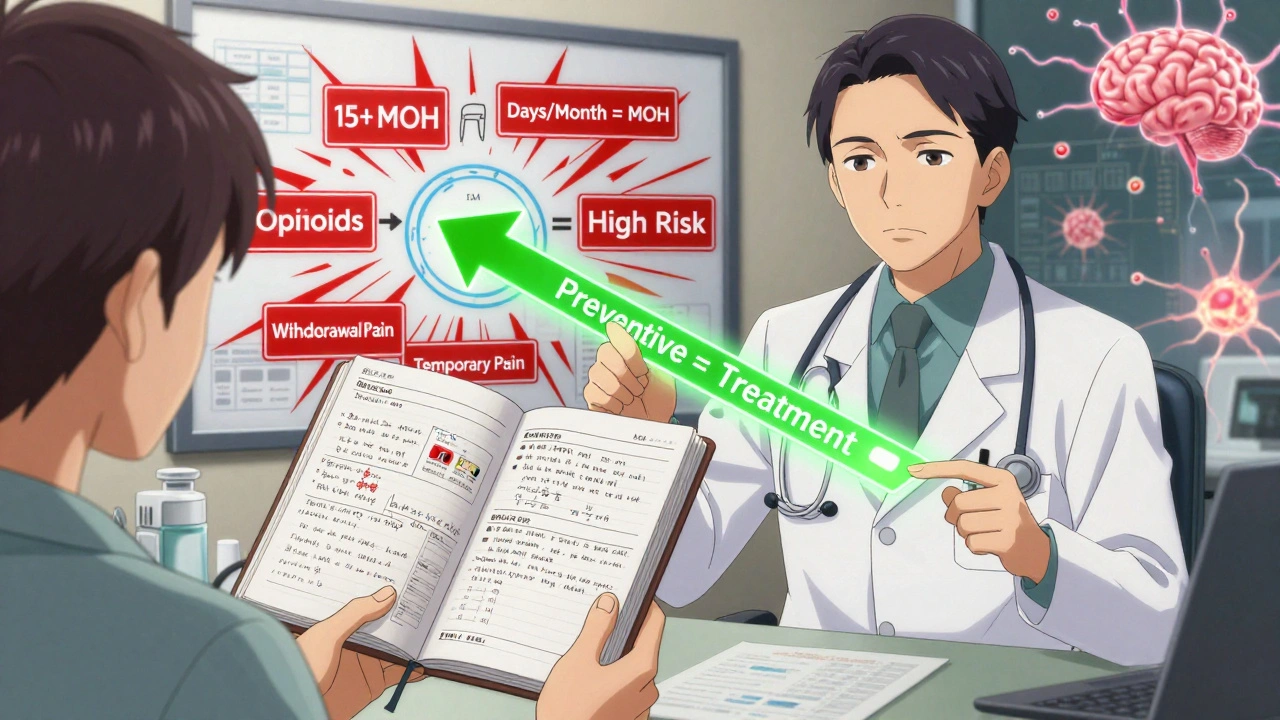
What Happens When You Stop?
Stopping the medication is the only cure. But it’s not easy.
Withdrawal symptoms are real-and intense. In one 2022 study of 350 patients, 92% had worse headaches during withdrawal. Other common symptoms:
- Nausea (68%)
- Vomiting (42%)
- Low blood pressure (29%)
- Insomnia, anxiety, restlessness
These symptoms usually peak within the first week and start to fade after two to four weeks. But the first few days? They’re brutal. That’s why many people give up and go right back to their pills.
Some patients need inpatient care-especially those using opioids or butalbital daily. But for most, outpatient withdrawal works if you have a plan.
How to Break the Cycle: A Realistic Plan
There’s no magic trick. But there is a proven path:
- Track your medication use. Write down every pill you take-name, dose, time, and reason. Use a calendar or app. You need at least four weeks of data before making changes.
- Choose your stopping method. For NSAIDs and triptans, stopping cold turkey often works. For opioids or butalbital, taper slowly under medical supervision. Abruptly quitting these can be dangerous.
- Use rescue meds wisely. During withdrawal, you might need one or two days of relief. Stick to a medication you haven’t overused-like acetaminophen (Tylenol), but only 2 days a week max.
- Start prevention right away. Don’t wait for withdrawal to end. If you have migraines, begin preventive treatment immediately. Topiramate, propranolol, or CGRP blockers like Aimovig or Nurtec can reduce headache frequency by 50-60%. Waiting increases your chance of relapse by 78%, according to Cleveland Clinic data.
- Give it time. Most people see improvement within 4 to 6 weeks. One Reddit user shared: “After 5 weeks off Excedrin, my headache days dropped from 28 to 9 per month.” That’s not luck-it’s science.
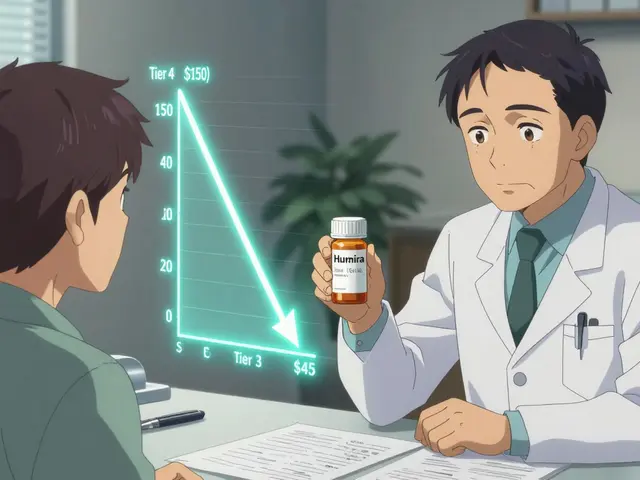
New Hope: Safer Alternatives
There’s good news on the horizon. A new class of migraine drugs called gepants (Ubrelvy, Nurtec ODT, Zavzpret) doesn’t seem to cause medication overuse headaches. Clinical trials show they’re just as effective as triptans-but without the rebound risk. They’re expensive ($750/month), but prescriptions for them grew 200% between 2021 and 2023 because doctors are finally recognizing their value.
Even newer is atogepant (Qulipta), approved by the FDA in January 2024 for preventive use in chronic migraine patients-including those with MOH. It’s taken daily and helps reduce both headache frequency and the urge to overuse acute meds.

Why Do Some Doctors Miss This?
MOH is underdiagnosed. Many patients are told they have “chronic migraine” and given more meds. But if you’re taking painkillers too often, that diagnosis is wrong. You have MOH.
There’s also confusion around NSAIDs. The American Headache Society says up to 15 days a month is fine. The European Headache Federation says 10 days is the limit. That gray area leaves patients guessing. If you’re taking ibuprofen or naproxen more than 10 days a month, you’re already at risk.
What You Can Do Today
If you’ve been having headaches more than 10 days a month and you’re using painkillers regularly:
- Stop blaming yourself. This isn’t weakness-it’s a physiological response.
- Start a headache diary. Write down every headache and every pill you take.
- Talk to your doctor about MOH. Bring your diary. Ask: “Could my headaches be caused by my medications?”
- Don’t quit cold turkey if you’re on opioids or butalbital. Ask for help.
- Ask about preventive options. Don’t wait until withdrawal is over.
MOH affects 1-2% of the population. That’s millions of people who think they’re stuck with daily headaches. But the good news? Once you stop the overused meds and start the right prevention, most people get their lives back.
What Happens If You Don’t Change Anything?
Left untreated, MOH gets worse. Headaches become more frequent, more intense, and harder to treat. You might start needing stronger drugs, higher doses, or even emergency care. The cycle keeps spinning-pain, pill, relief, pain again.
And here’s the kicker: the longer you wait, the longer it takes to recover. Studies show patients who delay withdrawal for over a year often need 6 to 12 months to fully recover. But those who act within 6 months? Many see major improvement in under two months.
You don’t have to live with daily headaches. The solution isn’t another pill. It’s stopping the ones you’re already taking-and replacing them with something that works long-term.
Can over-the-counter painkillers cause chronic headaches?
Yes. Even common OTC painkillers like ibuprofen, naproxen, and Excedrin can cause medication overuse headaches if taken 15 or more days a month for three months or longer. The risk is lower than with opioids or triptans, but it’s still real. Many people don’t realize their daily headache is caused by their daily aspirin or Advil.
How long does it take to recover from medication overuse headaches?
Most people see improvement within 4 to 6 weeks after stopping the overused medication. Withdrawal symptoms peak in the first week and gradually fade. Full recovery-where headaches return to their original episodic pattern-can take 2 to 3 months. Some patients with long-term overuse may need up to 6 months.
Is it safe to quit headache meds cold turkey?
It depends on the drug. For NSAIDs or triptans, stopping suddenly is usually safe. But for opioids, butalbital, or barbiturate combinations, abrupt withdrawal can cause seizures, severe blood pressure drops, or life-threatening symptoms. Always consult a doctor before quitting these medications. A gradual taper under medical supervision is required.
Why do I get worse headaches when I stop taking my painkillers?
Your brain has adapted to the medication. Over time, it changes how it processes pain signals and becomes dependent on the drug to stay balanced. When you stop, your nervous system goes into overdrive, causing rebound headaches. This isn’t addiction-it’s a neurological adaptation. It’s why headaches feel worse before they get better.
Can I ever use painkillers again after recovering from MOH?
Yes-but with strict limits. Most experts recommend using acute headache meds no more than 2 days per week. Use them only for true emergencies, not routine relief. Avoid opioids and butalbital entirely. Consider safer alternatives like gepants (Nurtec, Ubrelvy) if you have migraines. Keeping a headache diary helps you stay within safe limits.
Are there non-drug ways to manage headaches after stopping overused meds?
Absolutely. Behavioral therapies like cognitive behavioral therapy (CBT), biofeedback, and regular aerobic exercise have strong evidence for reducing headache frequency. Newer options include transcranial magnetic stimulation (TMS), which the Migraine Research Foundation is currently studying as a withdrawal aid. Sleep hygiene, stress management, and hydration also play key roles. These aren’t replacements for preventive meds-but they’re powerful supports.




i just started keeping a headache diary n i cant believe how much advil i was takin lol like 20 days a month?? no wonder my head never stopped hurtin 😅