Deprescribing Risk Assessment Tool
Assess Your Medication Risk
This tool helps identify potentially inappropriate medications based on your current prescriptions and health status. It's designed for older adults who take multiple medications.
Your Risk Assessment
Based on your responses, you have:
You may benefit from discussing deprescribing with your doctor. Consider asking:
- Which of these medications are still helping me?
- Are any of these linked to dizziness, confusion, or falls?
- Would it be safe to try stopping one for a few weeks?
Why Stopping Medications Can Be Healthier Than Taking Them
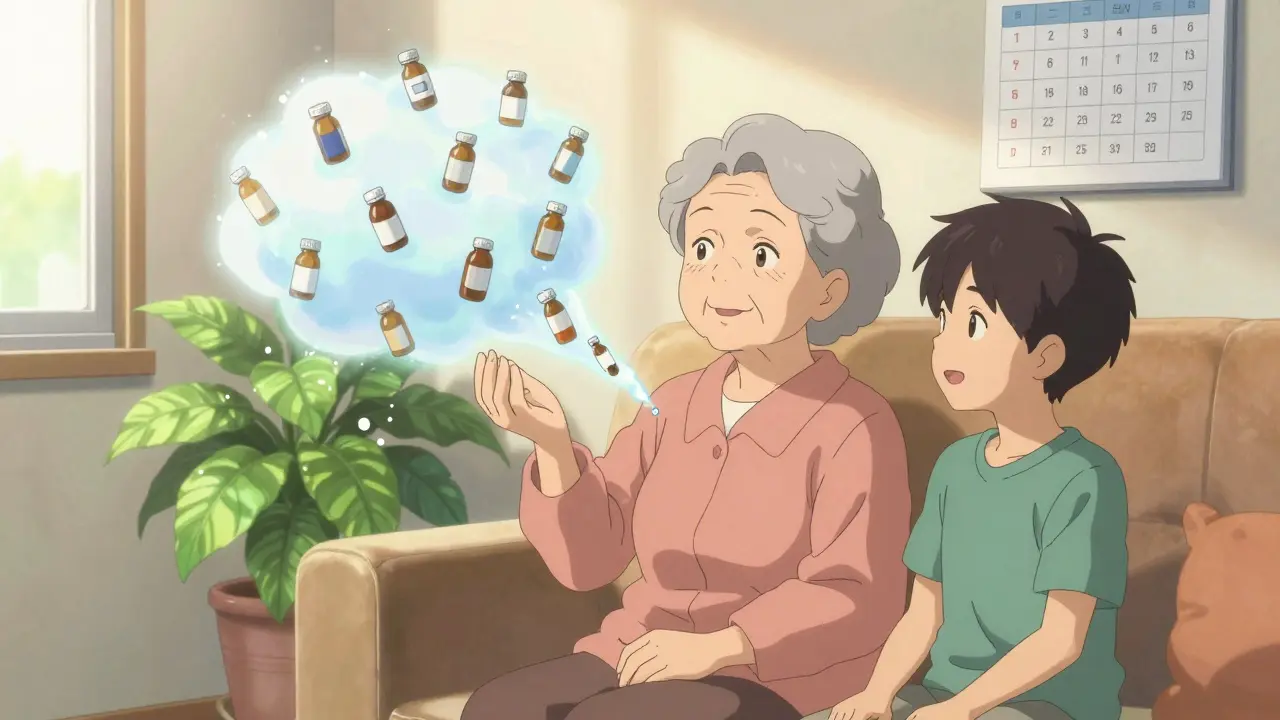
Most people assume more pills mean better care. But what if taking fewer medications actually makes you safer, healthier, and more in control? That’s the quiet revolution happening in geriatric medicine today - deprescribing. It’s not about stopping drugs randomly. It’s a careful, evidence-based process of removing medicines that no longer help - or worse, hurt.
Imagine an 82-year-old woman taking 12 medications daily: blood pressure pills, cholesterol drugs, diabetes meds, a sleep aid, a stomach acid reducer, and a painkiller. She’s not sick enough to need all of them, but no one ever asked if she still needed them. She’s tired all the time. She’s fallen twice in the last six months. Her doctor focused on treating each number - blood pressure, glucose, cholesterol - but never looked at the whole picture. That’s where deprescribing steps in.
What Exactly Is Deprescribing?
Deprescribing isn’t just cutting pills. It’s a structured clinical process defined by experts as evaluating whether the harms of a drug outweigh its benefits - based on the patient’s real-life function, life expectancy, and personal goals. The American Geriatrics Society calls it "the planned and supervised process of dose reduction or stopping of medication that might be causing harm, or no longer be of benefit."
This isn’t a new idea. But it’s only recently become a formal practice. The Canadian Deprescribing Guidelines Initiative launched in 2015, and since then, dozens of studies have shown it works - when done right. The goal? Reduce medication burden without sacrificing safety or quality of life. In fact, research shows that for older adults with multiple chronic conditions, fewer meds often mean fewer falls, less confusion, and better energy.
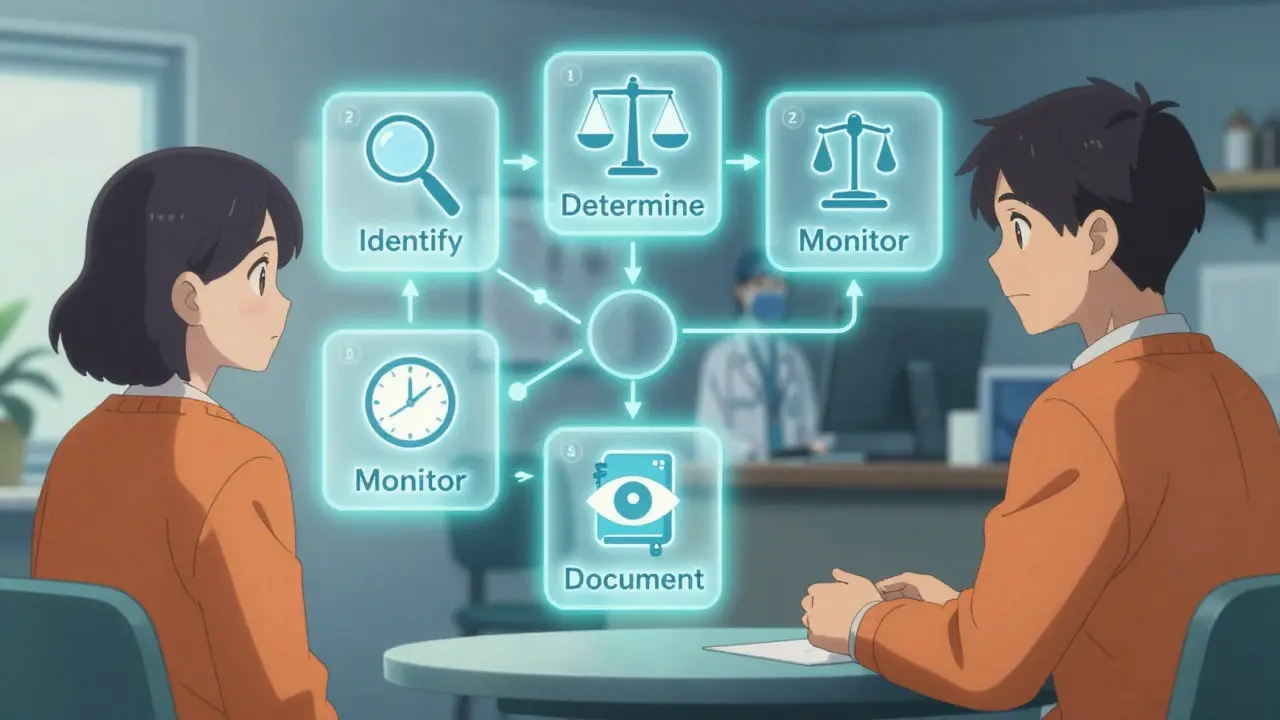
The Five Steps of Safe Deprescribing
Deprescribing isn’t guesswork. It follows five clear steps, just like starting a new drug:
- Identify potentially inappropriate medications - These are drugs with known risks for older adults, like benzodiazepines for sleep, proton pump inhibitors for heartburn used long-term, or anticholinergics that cause brain fog.
- Determine if the dose can be lowered or stopped - Not all meds need to be stopped cold turkey. Some can be reduced slowly. Others might be unnecessary if the original reason for taking them no longer applies.
- Plan a taper - Abruptly stopping certain drugs - like antidepressants or blood pressure meds - can cause withdrawal or rebound effects. A slow, monitored reduction is safer.
- Monitor for symptoms - After stopping a drug, watch closely. Does the patient feel better? Worse? Do old symptoms return? This step is critical and often skipped.
- Document everything - What was stopped? Why? What happened after? This record helps future providers avoid repeating mistakes.
One key rule: stop one drug at a time. If you remove five pills at once and the patient feels better, you won’t know which one helped. If they feel worse, you won’t know which one to bring back.
Who Benefits the Most?
Deprescribing isn’t for everyone. It’s most useful for:
- Older adults taking five or more medications (polypharmacy)
- Those with frailty, dementia, or advanced illness
- People who’ve had a recent fall, confusion, or dizziness
- Those on preventive drugs - like statins or aspirin - with no clear short-term benefit
- Patients on high-risk combinations, like multiple sedatives or drugs that affect the same organ system
Studies show that in nursing homes and home care settings, deprescribing reduces falls by up to 30%. In one trial, stopping sleeping pills in older adults improved balance and reduced dizziness within weeks - without worsening sleep.
What Does the Research Say About Outcomes?
Early studies were skeptical. Some claimed stopping meds didn’t change hospital visits or death rates. But those studies had flaws - short follow-up times, small groups, and outcomes measured only in numbers, not real-life results.
More recent, larger studies tell a different story. A 2023 review in JAMA Network Open analyzed 62 trials involving over 15,000 older adults. The results? Deprescribing reduced the average number of medications per person by about 1.5 pills. Sounds small? Think bigger: a primary care doctor with 2,000 patients could prevent over 140 unnecessary prescriptions annually just by applying deprescribing principles.
And the benefits go beyond numbers:
- Reduced risk of falls and fractures
- Improved mental clarity and alertness
- Lower rates of hospitalization
- Less digestive upset from acid reducers and laxatives
- Lower pharmacy costs - and fewer side effects
One patient, 78, stopped taking a daily antipsychotic for "agitation" linked to mild dementia. Within three weeks, her mood improved. She started talking more with family. She didn’t need the drug anymore - it was just masking the real issue: loneliness and lack of stimulation.
The Big Miss: Why Doctors Don’t Talk About It
Here’s the uncomfortable truth: most doctors don’t bring up deprescribing - and patients rarely ask for it.
A 2019 study by the American Academy of Family Physicians found that patients want to take fewer pills - but they assume their doctor knows best. They don’t want to seem ungrateful or question their care. So they stay on meds they don’t need.
Doctors, meanwhile, are pressured by guidelines that focus on starting treatments, not stopping them. They fear lawsuits if a condition returns. They’re overwhelmed. And they often don’t have the tools to know which meds to cut.
But change is coming. New point-of-care tools in electronic health records are now flagging high-risk prescriptions. One pilot program in family clinics cut inappropriate meds by 15% just by adding a simple alert during appointments.
How Patients Can Start the Conversation
If you or a loved one are on five or more medications, here’s how to begin:
- Ask: "Which of these meds are still helping me?"
- Ask: "Are any of these linked to dizziness, confusion, or falls?"
- Ask: "Would it be safe to try stopping one for a few weeks?"
- Bring a full list - including supplements and OTC drugs - to your appointment.
- Don’t stop anything on your own. Always work with your provider.
Resources like deprescribing.org offer free patient guides in plain language. They’ve been downloaded over half a million times - proof that people are ready for this conversation.
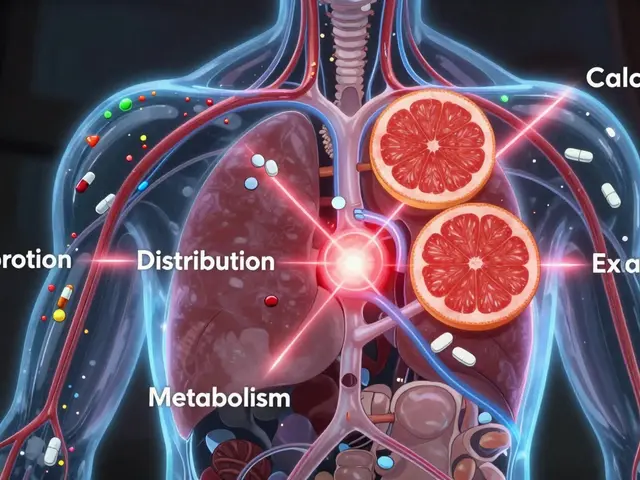
The Future: Personalized Deprescribing
Research is moving beyond "one-size-fits-all" guidelines. Scientists are now exploring how genetics affect drug metabolism. For example, some people break down benzodiazepines slowly - making them far more likely to fall. Others clear proton pump inhibitors quickly, making long-term use pointless.
Future tools may use AI to predict which drugs are most likely to cause harm for a specific person - based on age, kidney function, other meds, and even DNA. Trials are already testing these algorithms in real clinics.
As the U.S. population ages - with 20% expected to be over 65 by 2030 - deprescribing won’t be optional. It’ll be essential. The goal isn’t to eliminate all meds. It’s to make sure every pill you take still has a reason to be there.
Final Thought: Medications That Were Good Then Might Not Be Best Now
Medicine isn’t static. Your body changes. Your goals change. A pill that helped you after heart surgery five years ago might be doing nothing now - or worse, making you feel worse.
Deprescribing isn’t about giving up. It’s about choosing wisely. It’s about focusing on what matters: feeling well, staying safe, and living with dignity - not just ticking boxes on a lab report.
Is deprescribing safe?
Yes, when done properly. Studies show that stopping unnecessary medications under medical supervision is safe and often improves health. Withdrawal symptoms are rare and usually mild when tapering is used. The biggest risk is doing it without a plan - not doing it at all.
Can deprescribing cause health problems?
It can - but only if done carelessly. Stopping blood pressure or antidepressant meds suddenly can cause rebound effects. That’s why a slow taper and close monitoring are essential. The risks of staying on harmful meds - like falls, confusion, or kidney damage - are far greater than the risks of carefully stopping them.
Who should consider deprescribing?
Older adults taking five or more medications, especially those with frailty, dementia, recent falls, or unclear benefits from preventive drugs. It’s also important for people nearing end-of-life care, where the goal shifts from long-term prevention to comfort and quality of life.
Do I need to stop all my meds?
No. Deprescribing targets only those drugs that are no longer helpful or are causing harm. Many essential medications - like insulin for diabetes or heart meds after a stroke - should continue. The goal is balance, not elimination.
Why isn’t deprescribing more common?
Doctors are trained to prescribe, not stop. Guidelines reward starting treatments. Patients don’t ask. There’s no financial incentive. And until recently, there wasn’t enough data to support it. But that’s changing fast - with new tools, research, and patient demand driving adoption.
Can I use deprescribing if I’m not elderly?
Yes. While most research focuses on older adults, anyone on multiple long-term meds - especially if they have side effects or unclear benefits - can benefit from a review. Younger people on long-term painkillers, acid reducers, or sleep aids may also be candidates.


i dunno why everyone's actin like this is some big revelation. my grandma took 17 pills a day and we cut it to 4. she started walkin again. no magic. just common sense.
they call it deprescribing like it's a new app.