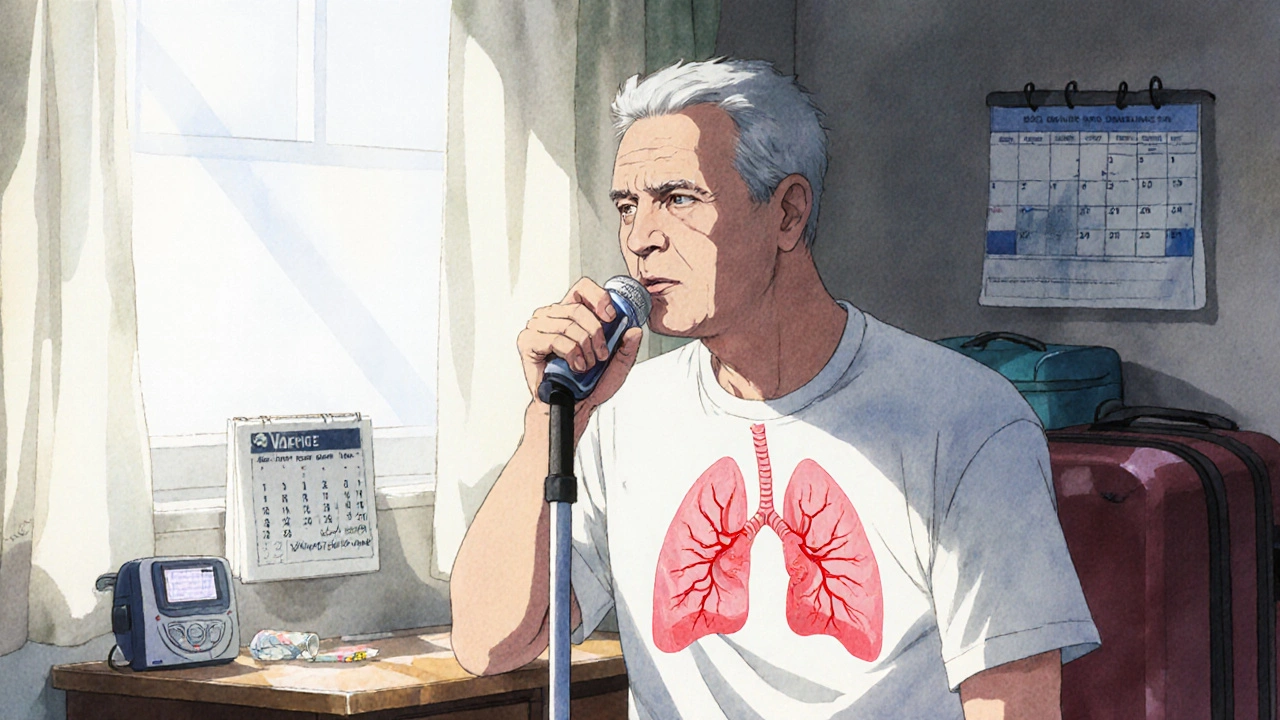
Chronic Obstructive Pulmonary Disease, or COPD, isn’t just a cough that won’t go away. It’s a progressive lung condition that slowly steals your ability to breathe normally - even during simple tasks like walking to the mailbox or getting dressed. By 2025, over COPD affects 380 million people worldwide, and it’s the third leading cause of death globally. Many don’t realize they have it until it’s advanced, because early symptoms are easy to ignore. If you’ve been told you’re "just out of shape" or "getting older," but you’re constantly winded, it’s worth digging deeper.
What Exactly Is COPD?
COPD isn’t one single disease. It’s an umbrella term for two main conditions: chronic bronchitis and emphysema. Chronic bronchitis means your airways are inflamed and produce too much mucus, making you cough daily. Emphysema damages the air sacs in your lungs, so they can’t properly exchange oxygen and carbon dioxide. Both make breathing harder over time.
The biggest cause? Smoking. About 85 to 90% of cases are directly linked to cigarette smoke. But it’s not just smokers. Long-term exposure to air pollution, chemical fumes, dust, or secondhand smoke can also trigger it. In some rare cases, a genetic condition called alpha-1 antitrypsin deficiency plays a role.
There’s no cure. But that doesn’t mean nothing can be done. The goal isn’t to reverse damage - it’s to slow it down, manage symptoms, and keep you active for as long as possible.
The Four Stages of COPD
COPD is staged using a system called GOLD (Global Initiative for Chronic Obstructive Lung Disease), updated in 2023. It’s not just about how bad your lungs look on a test - it’s also about how much your life is affected.
Doctors use a simple breathing test called spirometry to measure your FEV1 - how much air you can forcefully blow out in one second. That number is compared to what’s normal for someone your age, height, and gender. Here’s what each stage looks like in real life:
- Stage 1 (Mild): Your FEV1 is 80% or higher of predicted. You might have a persistent cough and clear mucus in the morning, but you probably don’t think it’s a big deal. Many people brush it off as "a smoker’s cough." You can still walk up stairs without stopping - but you might notice you’re slower than you used to be.
- Stage 2 (Moderate): FEV1 drops to 50-79%. Now, shortness of breath becomes noticeable during everyday activities - walking on level ground, carrying groceries, or doing light housework. You start to pause and catch your breath every few minutes. This is the stage where most people finally see a doctor. By now, lung function has dropped significantly, but there’s still room to make big improvements.
- Stage 3 (Severe): FEV1 falls to 30-49%. Breathing becomes a constant struggle. You might get winded putting on a shirt or taking a shower. Exacerbations - sudden flare-ups where symptoms get much worse - happen more often. You may need antibiotics or steroids several times a year. Your quality of life drops sharply. Many people start avoiding going out because they fear running out of breath.
- Stage 4 (Very Severe): FEV1 is below 30%, or below 50% with chronic low oxygen levels. Even sitting still can leave you gasping. Oxygen therapy becomes necessary most of the day. Simple tasks like brushing your teeth or talking for more than a few seconds become exhausting. You’re at high risk for life-threatening flare-ups, heart problems, and lung infections. This is the stage where options like lung volume reduction surgery or transplant are considered.
But here’s the catch: two people with the same FEV1 can feel totally different. One might be barely affected; another might be housebound. That’s why the GOLD system now also looks at your symptoms (using tools like the CAT score) and how often you’ve had flare-ups in the past year. This gives doctors a clearer picture of your actual risk and needs.
Treatment by Stage
Treatment isn’t one-size-fits-all. What works for someone in Stage 1 won’t be enough for someone in Stage 4.
Stage 1: Early Intervention Is Everything
If you’re diagnosed here, your biggest advantage is time. The single most powerful thing you can do is quit smoking - right now. Studies show quitting can cut the rate of lung function decline by half. That’s not a small win. It means you could live years longer with better breathing.
Medications at this stage are minimal. You’ll likely only need a short-acting inhaler like albuterol for when you feel tightness - not daily. But don’t skip the basics: get your flu shot every year. Get the pneumonia vaccine. Stay active. Walking 30 minutes a day helps your lungs work better, even if you’re short of breath.
Stage 2: Building a Routine
Now you’ll likely be prescribed a long-acting bronchodilator - either a LAMA (like tiotropium) or a LABA (like salmeterol). These keep your airways open for 12 to 24 hours. Many people use one daily, even when they feel fine.
Pulmonary rehabilitation is a game-changer here. It’s not just exercise - it’s a full program that teaches you how to breathe efficiently, manage anxiety, and pace your activities. People who complete it walk 54 meters farther on a 6-minute test, on average. That’s the difference between needing help to get to the bathroom and doing it alone.
And yes, vaccines matter more than ever. COPD patients are 5 times more likely to be hospitalized if they get the flu or COVID-19.
Stage 3: Managing Flare-Ups
At this stage, combination therapy is standard: a LAMA and LABA together, often in one inhaler. If you’ve had two or more flare-ups in the past year, your doctor may add an inhaled steroid. This reduces inflammation and lowers the chance of another attack.
Oxygen therapy may be introduced if your blood oxygen drops below 88% at rest. It’s not just for end-stage - many people in Stage 3 benefit from using oxygen during sleep or activity.
Exercise is still critical. Even if you’re tired, moving helps. Many patients start with seated exercises or walking with a portable oxygen tank. Physical activity doesn’t just improve breathing - it reduces depression and anxiety, which are common in advanced COPD.
Stage 4: Survival and Support
Continuous oxygen therapy - 15+ hours a day - is often required. The NOTT study showed this can improve survival by 44% in patients with severe low oxygen. But it’s not easy. Tanks are heavy. Portable units last only 4-6 hours. Many people feel trapped.
Lung volume reduction surgery removes damaged parts of the lung so the healthier parts can work better. It’s not for everyone, but for the right candidate, it can improve 2-year survival by 15%. Lung transplant is an option for those under 65 with very low FEV1 and no other major health issues.
At this stage, palliative care becomes part of the plan. It’s not giving up - it’s focusing on comfort, dignity, and quality of life. Pain, anxiety, and breathlessness are treated aggressively. Many patients find relief through non-drug methods like breathing techniques, music therapy, or counseling.
What’s New in COPD Treatment?
There’s real progress. In 2023, the FDA approved Breztri Aerosphere - the first single inhaler that combines three medications (LAMA, LABA, and steroid) for COPD. It’s simpler than juggling multiple devices.
Another promising drug, ensifentrine, is showing up in trials as a new type of bronchodilator that improves lung function by 13%. It could be available soon.
Digital tools are catching up too. The FDA-cleared Kyna COPD app uses AI to predict flare-ups 3-5 days in advance by tracking your symptoms, activity, and sleep. Early warning means you can start treatment before you’re hospitalized.
And research is moving toward personalized medicine. Scientists have identified over 80 genetic markers linked to how fast COPD progresses. In the future, your treatment may be tailored based on your DNA, not just your FEV1.

The Real Challenges
Even with all the advances, big problems remain.
Most people use their inhalers wrong. Studies show 70-80% make mistakes - pressing the canister too early, not holding their breath, or not cleaning the device. A single training session with a respiratory therapist can fix this. Ask for it.
Cost is another barrier. Spiriva (tiotropium) costs $350-$400 a month without insurance. Oxygen equipment can run $1,000+ per year. Medicare covers 80%, but you’re still on the hook for the rest. Many patients skip doses because they can’t afford them.
And then there’s the loneliness. One Reddit user wrote: "I used to love gardening. Now I can’t even stand for 5 minutes. My friends don’t understand why I don’t come over anymore." Social isolation is a silent killer in COPD. Support groups - like those run by the COPD Foundation - help. Talking to others who get it makes a difference.
What You Can Do Today
If you’re worried you might have COPD:
- Get a spirometry test. It’s quick, painless, and often covered by insurance.
- If you smoke, quit. Use nicotine patches, counseling, or apps like Smokefree.gov. Don’t try to quit cold turkey without support - success rates are low.
- Get vaccinated. Flu, pneumonia, and COVID-19 shots are non-negotiable.
- Start walking. Even 10 minutes a day. Build up slowly.
- Find a pulmonary rehab program near you. Ask your doctor. It’s the most effective non-drug treatment.
- Learn your inhaler technique. Ask your pharmacist to watch you use it.
If you’re already diagnosed:
- Track your symptoms. Use a notebook or app. Note when you feel worse - that helps your doctor adjust your plan.
- Know your exacerbation warning signs: more coughing, thicker mucus, increased shortness of breath, or swelling in your ankles.
- Don’t wait until you’re in crisis to call your doctor. Early action can keep you out of the hospital.
COPD doesn’t have to mean giving up. With the right care, many people live for years with good quality of life - even in Stage 3 or 4. The key is acting early, staying informed, and never stopping the fight to breathe better.
Can COPD be reversed?
No, COPD cannot be reversed. The lung damage from emphysema and chronic bronchitis is permanent. But quitting smoking and following a treatment plan can slow the progression dramatically. Many people stabilize their condition and live active lives for decades after diagnosis.
Is COPD the same as asthma?
No. Asthma is usually reversible with medication and often starts in childhood. COPD is progressive, usually caused by long-term smoking, and affects older adults. Some people have both - called asthma-COPD overlap syndrome (ACOS). Treatment for ACOS often includes inhaled steroids, which aren’t always needed in pure COPD.
How long can you live with COPD?
It varies widely. Someone with mild COPD who quits smoking and stays active can live for 20+ years. Someone with severe COPD and frequent flare-ups may have a shorter life expectancy. But survival isn’t just about stage - it’s about how well you manage it. Oxygen therapy, pulmonary rehab, and avoiding infections can add years.
Do I need oxygen all the time?
Only if your blood oxygen is consistently low - usually below 88% at rest. Not everyone with COPD needs it. If you do, your doctor will test you and prescribe the right flow rate. Many people only need it during sleep or activity, not 24/7. Portable oxygen devices now make it easier to stay mobile.
What’s the best way to prevent COPD flare-ups?
Avoid triggers: smoke, pollution, cold air, and crowds during flu season. Wash your hands often. Get vaccinated. Take your medications as prescribed - even when you feel fine. Learn your early warning signs and act fast. Many flare-ups can be stopped with a short course of steroids or antibiotics if caught early.
Can exercise make COPD worse?
No - avoiding exercise makes it worse. Being inactive causes muscles to weaken, which makes breathing harder. Pulmonary rehab teaches you how to exercise safely. Start slow: sit and breathe deeply, then stand and walk a few steps. Gradually increase. Many people find they can do more than they thought after just a few weeks.
Are there any new drugs on the horizon?
Yes. Ensifentrine, a new type of bronchodilator, showed strong results in 2023 trials. Single-inhaler triple therapy (like Breztri) is now standard for many. Researchers are also testing gene therapies and anti-inflammatory drugs targeting specific COPD subtypes. While not available yet, these could change treatment in the next 5-10 years.
What should I do if I can’t afford my COPD meds?
Talk to your doctor. Many drug companies offer patient assistance programs. Medicare Part D may help. Generic versions of some inhalers are now available. The COPD Foundation can connect you with resources. Never skip doses because of cost - there are options. Your health is worth fighting for.



Just read this through twice. The GOLD staging breakdown is spot-on-especially how it factors in symptom burden, not just FEV1. I’ve seen too many patients get dismissed as ‘just old’ when they’re actually in Stage 2. Pulmonary rehab saved my dad’s quality of life. Not magic, but it’s the closest thing we’ve got.