Clarithromycin Drug Interaction Checker
This tool checks for dangerous interactions between clarithromycin and common medications you may be taking. If you're prescribed clarithromycin, always check for interactions with your other medications.
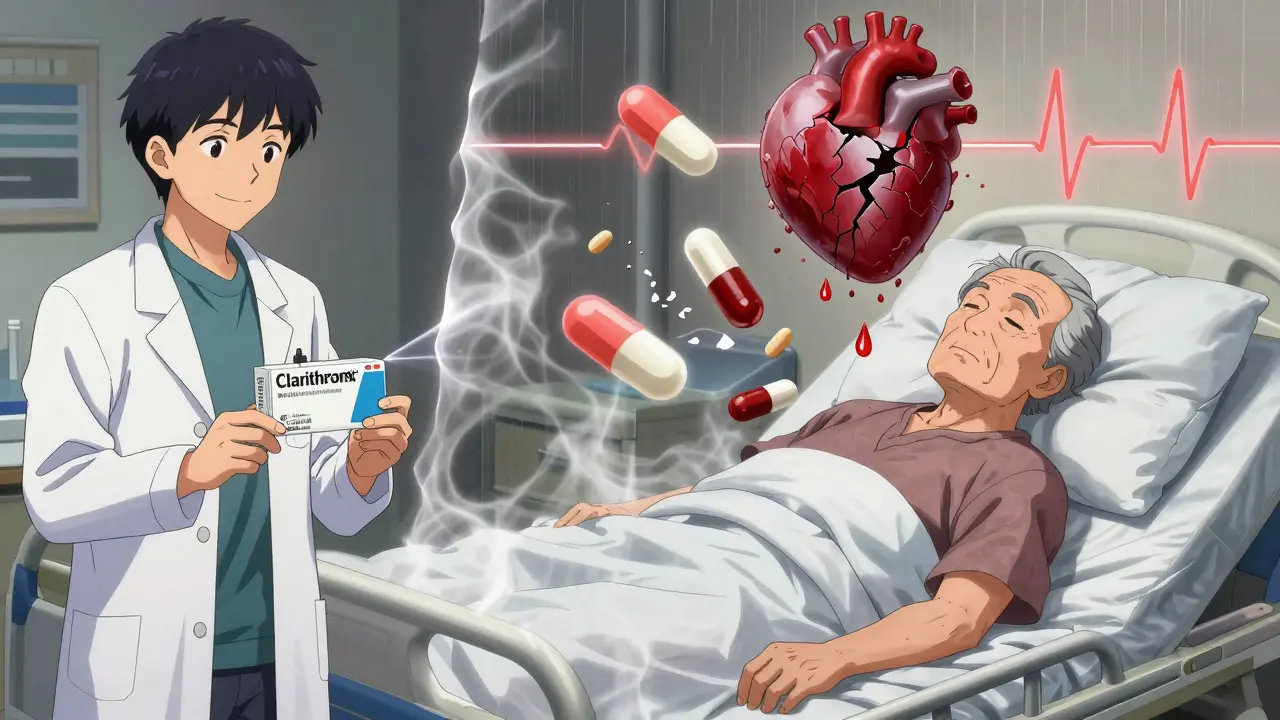
Clarithromycin is a powerful antibiotic, but it’s not just fighting bacteria-it’s also messing with your body’s ability to process dozens of other medications. If you’re taking clarithromycin, especially if you’re over 65 or on multiple prescriptions, you could be walking into a medical danger zone without even knowing it. The problem isn’t the infection you’re treating. It’s what happens when clarithromycin teams up with other drugs you’re already taking. This isn’t a rare side effect. It’s a well-documented, life-threatening risk that kills people every year.
Why Clarithromycin Is Different from Other Antibiotics
Most antibiotics don’t interfere much with other medications. Azithromycin, for example, is a close cousin of clarithromycin but doesn’t cause the same level of trouble. Clarithromycin, on the other hand, shuts down a key enzyme in your liver called CYP3A4. This enzyme is responsible for breaking down about half of all prescription drugs. When it’s blocked, those drugs don’t get cleared from your body. They build up. And when they build up too much, they become toxic.Think of it like a highway. CYP3A4 is the exit ramp that lets drugs leave your system. Clarithromycin slams that exit shut. Suddenly, everything else on the road-statins, blood pressure meds, gout pills-gets stuck. And the longer they’re stuck, the more damage they cause.
The Deadliest Combination: Clarithromycin and Colchicine
If you take colchicine for gout or pericarditis, you need to hear this: never take clarithromycin with it. This is not a "be careful" warning. This is a "you could die" warning.Colchicine is a drug with a very narrow safety margin. It works at low doses, and just a little extra can poison you. When clarithromycin blocks CYP3A4, colchicine levels in your blood can jump by more than 280%. That’s not a typo. One study showed that after just seven days of clarithromycin, a single dose of colchicine became 3.8 times more potent in the body.
What happens next? Severe diarrhea, vomiting, muscle weakness, kidney failure, and rhabdomyolysis-the breakdown of muscle tissue that can shut down your kidneys. In documented cases, people have died within two weeks of starting clarithromycin while still taking their regular colchicine dose. The FDA has recorded 58 serious or fatal cases of this interaction as of 2020, and experts believe the real number is much higher because many cases go unreported.
One real case involved a 76-year-old woman with chronic gout. She got a respiratory infection. Her doctor prescribed clarithromycin. She kept taking her 0.6 mg colchicine daily. Eleven days later, she was dead. Her body couldn’t handle the drug overload.
Statins: The Silent Killer
If you’re on a statin to lower cholesterol, clarithromycin could be turning it into a muscle-destroying toxin. Simvastatin and lovastatin are the worst offenders. Atorvastatin isn’t safe either, though it’s slightly less risky.When these statins mix with clarithromycin, your risk of rhabdomyolysis skyrockets. Muscles break down. Myoglobin floods your bloodstream. Your kidneys can’t filter it. You end up in the ICU needing dialysis.
One documented case involved a 68-year-old man on 40 mg of simvastatin daily. He started clarithromycin for bronchitis. Within 72 hours, he was in the hospital with muscle pain, dark urine, and kidney failure. He needed intensive care and dialysis to survive.
The American College of Clinical Pharmacy says if you absolutely must take both, reduce the statin dose by 50-75% and monitor for muscle pain. But the safest move? Swap clarithromycin for azithromycin-or switch your statin to pravastatin or rosuvastatin, which are less affected by CYP3A4 inhibition.

Heart Medications: A Recipe for Arrhythmia
Clarithromycin doesn’t just raise drug levels-it also prolongs your heart’s QT interval. That’s the time between heartbeats. If it gets too long, your heart can go into a deadly rhythm called torsades de pointes.This risk is worse if you’re already on other QT-prolonging drugs. Calcium channel blockers like verapamil, diltiazem, and amlodipine are common culprits. So are antiarrhythmics like amiodarone and sotalol. Even some antidepressants and antifungals can add to the danger.
The American Heart Association says clarithromycin increases the risk of torsades de pointes by 2.7 times compared to antibiotics that don’t affect the QT interval. If you have a history of heart rhythm problems, or if you’re on multiple heart meds, clarithromycin could be the trigger that sends you into cardiac arrest.
Warfarin, Digoxin, and Other Hidden Risks
Warfarin, a blood thinner, is another dangerous combo. Clarithromycin can make warfarin stick around longer, increasing your risk of dangerous bleeding-even if your INR was stable before. Digoxin, used for heart failure and atrial fibrillation, can also spike to toxic levels. Symptoms include nausea, confusion, vision changes, and irregular heartbeat.Even epilepsy medications like carbamazepine and theophylline (used for asthma) can become dangerous. Clarithromycin can make them build up to seizure-inducing or heart-stopping levels.
The Institute for Safe Medication Practices calls the clarithromycin-colchicine interaction a "Category A" high-alert combination-the same level as insulin and heparin. That means a mistake here isn’t just possible. It’s expected to cause serious harm.
Who’s Most at Risk?
You don’t have to be old to be in danger. But if you’re over 65, you’re far more vulnerable. Studies show 42% of seniors taking clarithromycin are also on at least one drug that interacts with it. That’s more than 4 in 10. The Beers Criteria, used by doctors nationwide, explicitly says: avoid clarithromycin in older adults taking CYP3A4 substrates.People with kidney disease are also at higher risk. The European Medicines Agency says clarithromycin and colchicine should never be combined in patients with severe kidney impairment. Their bodies can’t clear either drug, so levels rise even faster.
And here’s the kicker: many patients don’t know they’re at risk. They see clarithromycin as a simple antibiotic. They don’t think to mention their gout pill, cholesterol med, or blood pressure tablet. Pharmacists often catch these errors-but not always.
What Should You Do?
If your doctor prescribes clarithromycin:- Stop. Don’t fill the prescription yet.
- Make a list of every medication you take-including vitamins, supplements, and over-the-counter drugs.
- Ask your doctor: "Is this the safest antibiotic for me?" and "Could this interact with anything I’m already taking?"
- Ask your pharmacist to run a drug interaction check.
- If you’re on colchicine, a statin, a heart med, or warfarin, insist on azithromycin instead.
Azithromycin works just as well for most infections-pneumonia, sinus infections, strep throat-and it doesn’t wreck your other meds. It’s the safer choice, especially if you’re on more than three medications. In fact, since 2015, azithromycin has replaced clarithromycin as the #1 macrolide antibiotic in the U.S., not because it’s stronger, but because it’s safer.
The Bigger Picture: Why This Keeps Happening
You’d think hospitals and pharmacies would have systems to catch this. They do. But they’re not foolproof. A 2022 Medscape case showed a pharmacist stopping a fatal interaction between clarithromycin, colchicine, and rivaroxaban-but only because she double-checked the chart. That’s not a system. That’s luck.The FDA added a boxed warning to clarithromycin labels in 2023. That’s the strongest warning they give. It says: "Concomitant use has resulted in fatal and near-fatal colchicine toxicity." But warnings don’t stop mistakes. Education does. And most patients aren’t told. Most doctors assume the pharmacy will catch it. Most pharmacists assume the doctor knows.
Clarithromycin isn’t going away. It’s still used for serious infections like Mycobacterium avium complex in people with HIV. But for everyday infections? It’s outdated. And dangerous.
The CDC’s Dr. Jane Smith said in 2023 that clarithromycin will likely be relegated to niche use within the next decade-just like erythromycin was in the 90s. The writing’s on the wall. If you’re prescribed clarithromycin, ask: is this really necessary? Is there a safer option?
Your life might depend on it.
Can I take clarithromycin if I’m on a statin?
Avoid clarithromycin if you’re taking simvastatin or lovastatin-they can cause life-threatening muscle damage. Atorvastatin is less risky but still dangerous. Switch to pravastatin or rosuvastatin, or ask for azithromycin instead. Never combine clarithromycin with a statin without close monitoring from your doctor.
Is azithromycin always a safer alternative?
Yes, for most common infections. Azithromycin doesn’t significantly inhibit CYP3A4, so it rarely causes dangerous interactions. It’s now the preferred macrolide for patients on multiple medications. The only exceptions are rare infections like Mycobacterium avium complex, where clarithromycin is still essential.
How long do clarithromycin interactions last?
Clarithromycin’s effect on CYP3A4 can last for days after you stop taking it. The enzyme doesn’t recover immediately. That means if you stop clarithromycin and then start a statin or colchicine a few days later, you’re still at risk. Wait at least 5-7 days after finishing clarithromycin before restarting any interacting drug.
What should I do if I’ve already taken clarithromycin with colchicine?
Stop taking colchicine immediately and call your doctor or go to the ER. Symptoms of toxicity include severe diarrhea, vomiting, muscle pain, weakness, or dark urine. Don’t wait. This can become fatal within days. Bring your medication list with you.
Are there any safe antibiotics if I’m on multiple medications?
Azithromycin is the safest macrolide. Amoxicillin, doxycycline, and cephalexin are also low-risk options for many infections. Always check with your pharmacist or doctor before starting any new antibiotic if you’re on three or more medications.





I had no idea clarithromycin could mess with statins like that. My grandma was on simvastatin and got this antibiotic last winter-thank god her pharmacist caught it before she filled it. Scary stuff.