Most people don’t realize their kidneys are failing until it’s too late. That’s because chronic kidney disease (CKD) doesn’t scream for attention. No sharp pain. No fever. Just a slow, quiet decline that slips under the radar-until it doesn’t. By the time symptoms like fatigue, swelling, or nausea show up, up to 80% of kidney function may already be gone. The good news? CKD doesn’t have to sneak up on you. With the right tests and awareness, you can catch it early, slow it down, and even prevent dialysis.
What Exactly Is Chronic Kidney Disease?
Chronic kidney disease isn’t just one thing. It’s a group of conditions where your kidneys are damaged and can’t filter blood the way they should. This damage lasts for at least three months. The kidneys don’t just remove waste-they balance fluids, control blood pressure, make red blood cells, and keep your bones strong. When they start to fail, everything else starts to unravel.
The current standard for defining CKD comes from KDIGO, the global kidney health group. Their 2012 guidelines are still used today because they work. CKD isn’t just about how well your kidneys filter-it’s about damage and function together. You can have normal filtering power but still have CKD if there’s evidence of harm-like protein in your urine or structural changes seen on an ultrasound.
The Six Stages of CKD: It’s Not Just One Number
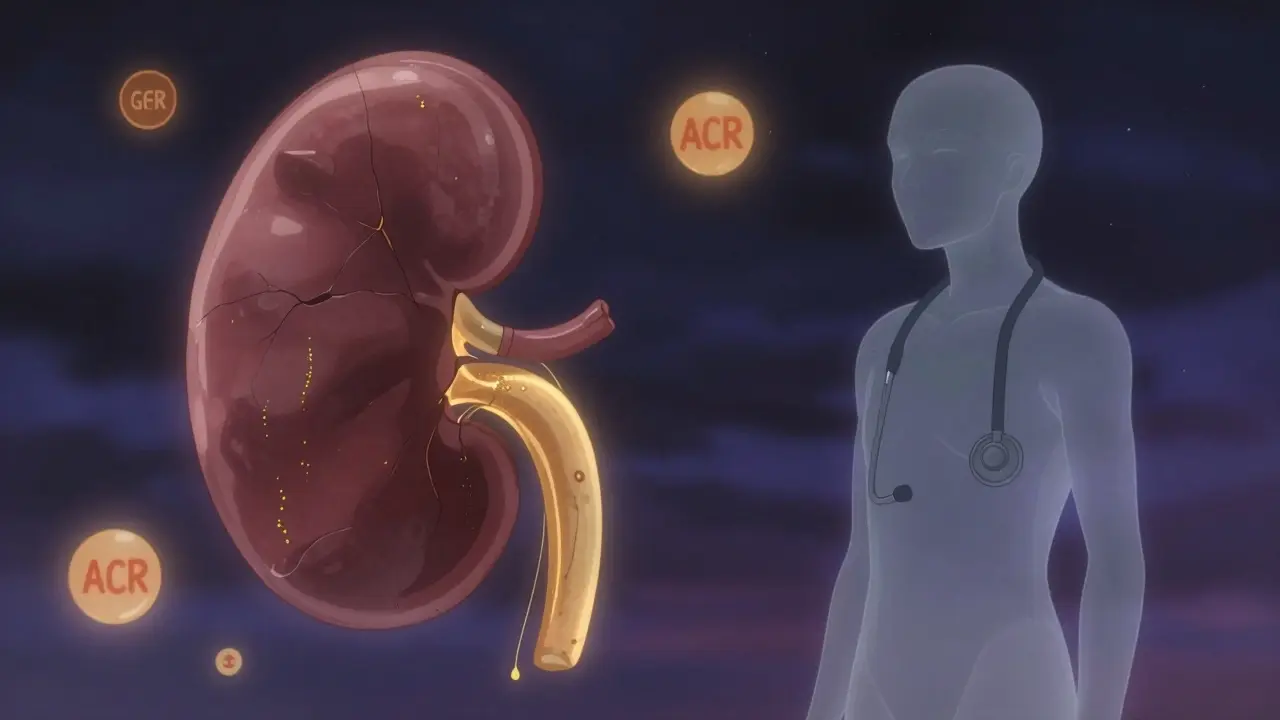
Doctors don’t just look at one number to judge your kidneys. They use two key measurements: eGFR and albuminuria. Together, they give a full picture of where you stand.
eGFR stands for estimated glomerular filtration rate. It’s a calculation based on your blood creatinine level, age, sex, and race. Since 2021, race has been removed from the equation because it led to inaccurate results. A normal eGFR is 90 or above. But here’s the twist: you can have an eGFR of 95 and still have CKD if your urine test shows protein.
Albuminuria measures how much protein-specifically albumin-is leaking into your urine. Healthy kidneys don’t let much pass. When they do, it’s a red flag. The test is done with a simple first-morning urine sample, measuring albumin-to-creatinine ratio (ACR). The results fall into three categories:
- A1: Less than 3 mg/mmol (normal or mildly increased)
- A2: 3 to 30 mg/mmol (moderately increased)
- A3: More than 30 mg/mmol (severely increased)
Now, combine eGFR with albuminuria, and you get the real picture. Here’s how the stages break down:
| Stage | eGFR (mL/min/1.73m²) | What It Means | Albuminuria Risk |
|---|---|---|---|
| G1 | 90 or higher | Kidneys look normal, but there’s damage | A2 or A3 = high risk |
| G2 | 60-89 | Mild reduction in function | A2 or A3 = moderate risk |
| G3a | 45-59 | Mild to moderate loss | A3 = high risk of fast decline |
| G3b | 30-44 | Moderate to severe loss | 2.6x higher chance of reaching kidney failure |
| G4 | 15-29 | Severely reduced function | Preparation for dialysis or transplant needed |
| G5 | Less than 15 | Kidney failure | Dialysis or transplant required |
Here’s what matters most: someone with G3a and A3 has a much higher chance of losing kidney function fast than someone with G3a and A1. That’s why both numbers are needed. One without the other is like trying to drive with one eye closed.
Why Early Detection Changes Everything
Most people with CKD don’t know they have it. The National Institute of Diabetes and Digestive and Kidney Diseases says 90% of those with CKD are undiagnosed. Why? Because early stages have no symptoms. You feel fine. You sleep fine. You go to work. But your kidneys are quietly leaking protein and struggling to filter.
Think about it this way: if you found out your blood pressure was high at 45, you’d start changing your diet, exercising, maybe taking medication. You’d avoid a heart attack. CKD is the same. Catch it early, and you can slow it down-sometimes stop it.
Studies show that if you catch CKD at Stage G1 or G2 and manage it properly, you reduce your risk of needing dialysis by 25-30%. That’s huge. The tools are simple: a blood test for creatinine and a urine test for albumin. Both are cheap, fast, and often done during routine check-ups.
But here’s the catch: many doctors don’t order them unless you’re diabetic or hypertensive. And even then, they might not follow up. That’s why so many people get diagnosed late. One patient in Melbourne told me, “I didn’t know I had diabetes until my kidney test came back. My kidneys were already damaged.”
Who Should Get Tested-and How Often
You don’t need to be sick to get tested. If you’re at risk, you should be checked regularly. Here’s who needs it:
- People with diabetes (type 1 or type 2)
- People with high blood pressure
- People with heart disease
- People with a family history of kidney failure
- People over 60
- People of African, Native American, or Hispanic descent
For those with risk factors, testing should happen at least once a year. If you’re diabetic, get both tests every year. If your eGFR drops more than 5 mL/min/year, that’s a red flag. That’s rapid decline. You need a nephrologist.
And don’t wait for symptoms. By the time you feel tired, puffy, or nauseous, your kidneys are already in trouble. The only way to catch it early is to test.
The Real Danger: Overdiagnosis and Underdiagnosis
There’s a debate in nephrology circles right now. Some experts say we’re diagnosing too many people-especially older adults. An eGFR of 55 in a 75-year-old might just be normal aging. Their kidneys have been working for 75 years. They’re not failing-they’re just older.
Labeling someone with CKD when they’re not at risk can cause unnecessary stress. A UK study found 22% of people diagnosed with Stage G2 felt anxious, even though their kidneys were stable. That’s why some doctors now suggest calling it “mildly reduced kidney function” instead of CKD for people over 70 with no protein in their urine.
But the bigger problem is underdiagnosis. People with diabetes and high blood pressure are the most at risk-and they’re the least likely to be tested. A Cleveland Clinic study showed that when clinics started using electronic alerts for low eGFR and high urine protein, diagnosis rates jumped from 42% to 79% in just 18 months.
The solution? Systematic screening. Not waiting for symptoms. Not waiting for patients to complain. Just testing the right people, regularly.
What Happens If You’re Diagnosed Early
If you’re caught in Stage G1-G3a, the game changes. You’re not on dialysis. You’re not in crisis. You’re in control. Here’s what works:
- Control your blood pressure. Target under 130/80. ACE inhibitors or ARBs are often prescribed-not just for blood pressure, but to protect your kidneys.
- Manage your blood sugar. If you’re diabetic, HbA1c under 7% cuts kidney damage risk by 30%.
- Reduce salt. Less than 2,300 mg a day. Avoid processed foods.
- Stop smoking. Smoking speeds up kidney damage.
- Avoid NSAIDs. Ibuprofen, naproxen-they hurt kidneys over time.
- Stay hydrated. But don’t overdo it. Water helps, but too much can strain weak kidneys.
And here’s the kicker: if you have protein in your urine (A2 or A3), taking an ACE inhibitor can reduce your risk of progressing to Stage G4 by 37%. That’s not a guess. That’s from the SPRINT trial. It’s real. It works.
The Future: AI, Genetics, and Better Tools
The tools are getting smarter. In 2023, the FDA approved the first AI tool-AION nephroTM-that predicts your kidney function decline over two years with 88.7% accuracy. It looks at 27 factors: your age, blood pressure, lab results, medications, even your BMI.
And it’s not just AI. Researchers are now using genetic scores to predict who will lose kidney function fast. In a 2023 study, they identified 17 gene variants that, when combined, could predict progression with 92% accuracy. This isn’t science fiction. It’s happening now.
Point-of-care eGFR machines are also becoming common. Instead of waiting days for a lab result, your doctor can get your eGFR in 20 minutes during your visit. That means faster decisions, fewer missed cases.
The goal? Catch CKD before it catches you. And we’re getting closer.
What You Can Do Right Now
You don’t need to wait for a crisis. Here’s your action plan:
- If you have diabetes, high blood pressure, or are over 60, ask your doctor for an eGFR and urine ACR test-now.
- If your eGFR is below 60 and you have protein in your urine, don’t ignore it. See a nephrologist.
- If your numbers are normal, get tested every year.
- If you’re on blood pressure or diabetes meds, make sure they’re protecting your kidneys-not just your heart.
- Don’t wait for symptoms. If you feel fine, that’s a good sign. But it doesn’t mean your kidneys are fine.
Chronic kidney disease doesn’t have to be a death sentence. It can be a warning. And warnings are meant to be heeded-not ignored.
Can you have chronic kidney disease without symptoms?
Yes, absolutely. In fact, most people do. CKD is called a "silent disease" because it often causes no symptoms until it’s advanced. By the time you feel tired, swollen, or nauseous, you may have already lost 70-80% of kidney function. That’s why testing-especially for people with diabetes, high blood pressure, or a family history-is critical. A simple blood and urine test can catch it years before symptoms appear.
Is CKD the same as kidney failure?
No. CKD is a broad term that covers all stages of kidney damage, from mild to complete failure. Kidney failure is Stage G5, where the kidneys can no longer support life without dialysis or a transplant. Most people with CKD never reach kidney failure. With early detection and proper care, many people stabilize their condition and live for decades without needing dialysis.
Does having protein in my urine mean I have kidney disease?
Not necessarily-but it’s a strong warning sign. Protein in the urine (albuminuria) is one of the earliest signs of kidney damage. But it can also happen temporarily due to infection, fever, intense exercise, or dehydration. That’s why doctors require two abnormal tests at least 90 days apart before diagnosing CKD. One positive test doesn’t mean you have it. Two do.
Can lifestyle changes reverse chronic kidney disease?
You can’t reverse scarring, but you can stop or slow the damage. If you’re in Stage G1-G3a and make changes-controlling blood pressure, managing diabetes, reducing salt, quitting smoking-you can preserve what’s left. Some people even see their eGFR improve slightly by stabilizing their health. The goal isn’t to fix the damage-it’s to prevent more.
Why is eGFR calculated differently now?
Older formulas included race as a factor, assuming Black patients had higher muscle mass and thus higher creatinine levels. This led to underestimating kidney damage in Black patients. The 2021 CKD-EPI equation removed race entirely, using only age, sex, and creatinine. This made the calculation fairer and more accurate for everyone. If your eGFR was calculated before 2021, it may have been artificially inflated.
Should I be worried if my eGFR is 58?
It depends. An eGFR of 58 falls into Stage G3a, which means mild to moderate kidney function loss. But if your urine test shows no protein (A1) and your numbers have been stable for years, it might just be age-related. If your eGFR dropped quickly-from 70 to 58 in a year-or if you have protein in your urine, that’s a red flag. Talk to your doctor. Don’t panic. But don’t ignore it either.
Can I still live a normal life with CKD?
Yes, absolutely. Many people with Stage G1-G3 CKD live full, active lives for decades. The key is managing the underlying causes-diabetes, high blood pressure, obesity-and avoiding things that harm kidneys, like NSAIDs and smoking. People who catch it early and take action often outlive those who never knew they had it.