Why So Many Are Looking for a Substitute for Nexium 40 mg
It’s wild how much time people spend scanning pharmacy aisles, holding boxes of heartburn pills, and silently asking, “Will this even work for me?” Nexium 40 mg (that purple pill) isn’t the only game in town—especially with prescriptions harder to get and rising costs squeezing everyone. About one in five Aussies wrestle with heartburn at least once a week. If that’s you, you already know the burning sensation. Some of us just swallow it down with antacids and hope for the best. Others have tried Nexium, or rather, its generic sidekick, esomeprazole. It’s been a staple for GERD, acid reflux, and peptic ulcers, cutting acid production deep down at the source. But there’s a catch: long-term use can deliver a few headaches (sometimes literally)—think headaches, low magnesium, vitamin deficiencies, and even higher risk for gut infections. Recent regulatory changes mean regular folks have to jump through more hoops to get that 40 mg strength from behind the pharmacy counter. So, what’s next?
There’s a demand for reliable, easily accessible substitutes that actually shut down the misery without making you feel like a medical guinea pig. The OTC shelves here in Melbourne (and honestly worldwide) are bursting with choices. You see antacids, H2 blockers, and down-dosed PPIs all standing shoulder-to-shoulder. So, which over-the-counter substitute for Nexium 40 mg will calm raging heartburn, and which are just fancy mints? Picking the right replacement isn’t just about cost or convenience—it’s about getting back to enjoying your morning coffee without dreading the burn. Below, you’ll find brutally honest insights about what works (and what doesn’t), how much to take, and what to watch for.
The Main OTC Heartburn Players: Antacids, H2 Blockers, and Lower-Dose PPIs
Cracking open the world of over-the-counter acid relief is like scrolling through a streaming service—endless options, but most aren’t blockbusters. For years, antacids were the go-to: chews and tablets that kick in within minutes, breaking up acid like a chemical fire extinguisher. Tums, Mylanta, and Gaviscon all fall into this camp. They’re ideal if heartburn crashes in occasionally, but their effects vanish fast—half an hour later, you’re often right back on the struggle bus.
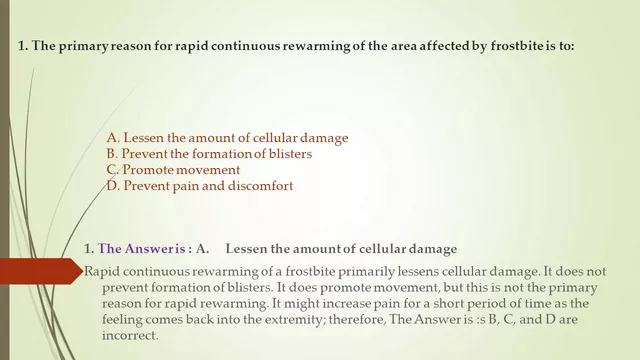
Then there’s the H2 blockers—famotidine (Pepcid) is the current top pick, with old-school reliables like ranitidine phased out due to contamination issues. These work by blocking histamine in the stomach lining, dialing down acid for hours instead of minutes. For most, one 10–20 mg famotidine tablet before a spicy meal or before bed keeps heartburn in check for up to 12 hours. Still, they don’t shut down acid as completely as Nexium or other PPIs.
Speaking of PPIs, a few are available OTC, though rarely in the 40 mg strength you recognize from your Nexium script. The big names are omeprazole (Prilosec), lansoprazole (Prevacid), and esomeprazole (Nexium 20 mg here in Australia). They work by actually deactivating the proton pumps that fuel stomach acid on a cellular level. These need to be taken daily—preferably 30–60 minutes before breakfast—for full effect. Half doses (20 mg vs. 40 mg) are usually the OTC standard because higher doses increase the risk of side effects if you self-treat for more than two weeks.
Here’s a snapshot of how they stack up:
| Type | Common Brands | Onset | Lasts | Drawbacks |
|---|---|---|---|---|
| Antacids | Tums, Mylanta, Gaviscon | 5-10 min | 30-60 min | Short-lived, not for severe cases |
| H2 Blockers | Pepcid, Tagamet | 30-60 min | 6-12 hrs | Less effective with tolerance, not instant |
| OTC PPIs | Nexium 20 mg, Omeprazole, Prevacid | 1-4 days for max effect | 12-24 hrs each dose | Slower start, side effects, dose limits |
That table might look straightforward, but those differences change everything when you’re trying to match your old Nexium results with an OTC swap. It’s not just about acid suppression numbers—how quick you need relief, how often symptoms hit, and your other health issues all steer the decision. Don’t get sucked in by advertising hype about “complete relief”—most folks benefit most from a combo approach, not just one product. (Hot tip: If antacids work, but only until two in the morning, try an H2 blocker at night; for daily misery, switch to a PPI, even the OTC strength one.)
OTC Dosing Strategies: Getting It Right Without a Prescription
Getting the dose right means the difference between feeling like you can finally eat your favorite meals again and dealing with restless, burning nights. First up: antacids. There’s barely any mystery here. Take as soon as heartburn shows up (or just before that heavy meal), but don’t double up thinking you’re stacking effectiveness—it doesn’t work that way. The main risk? Too much can lead to constipation or diarrhea depending on the ingredients, not to mention a riskier business for kidneys if you overdo it.
For H2 blockers—famotidine in particular—the most common dose is 10 or 20 mg per tablet, usually once or twice daily. If you know heartburn will hit (say, pizza night or dinner with Indian takeaway), pop one right before the first bite. If you’re already burning, you can still take one, but relief might come slower. Avoid upping the dose unless a doctor gives you the green light. And if you need it longer than two weeks, get checked out. Frequent or severe symptoms can point to something nastier, like an ulcer.
Now for the heavyweight class: OTC PPIs like esomeprazole (20 mg). These are meant for a 14-day course—swallow the pill whole (never crush it) first thing in the morning before food, every day. Why morning? That’s when those proton pumps in your stomach are most active, and the medicine has the best shot at shutting down acid before it hits your throat or chest. It can take two to four days for maximum effect, so don’t give up if day one doesn’t fix everything. And don’t mix and match PPIs unless a doctor tells you. Go past two weeks? See a healthcare professional to rule out anything serious.
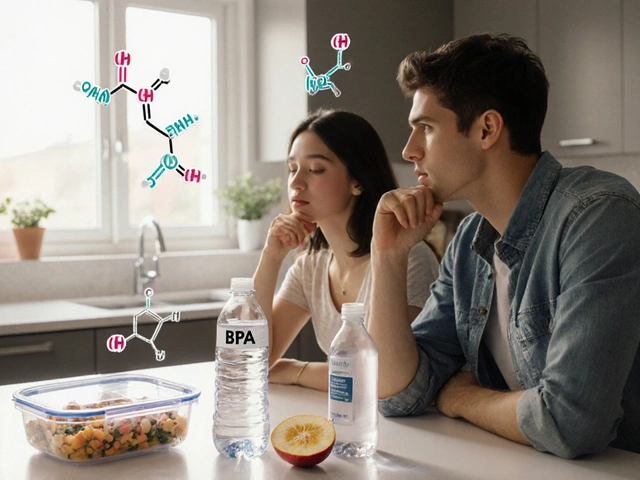
It’s tempting to chase that familiar Nexium 40 mg kick with double doses of the 20 mg OTC version. Don’t. Too much PPI can strip away essential stomach acids, leaving you vulnerable to gnarly infections like C. diff or even bone mineral loss if you stay on it months at a time. And never use these as an allergy workaround—people with true PPI allergies should try non-PPI alternatives instead of piling on antacids or H2 blockers out of desperation.
A key trick that isn’t on the label: Pair an antacid with an H2 blocker for breakthrough heartburn, but space them out. Take the antacid first (for fast relief), then the H2 blocker about 30–60 minutes later for staying power. Just don't take an antacid immediately before a PPI; that'll mess with absorption.
Comparing Safety and Side Effects: What to Watch Out For
Let’s be blunt: no heartburn treatment is risk-free, even if it’s on the supermarket shelf. Antacids sound harmless, but heavy and frequent use of calcium-based ones can cause kidney issues and weirdly enough, actually make heartburn worse (the 'rebound' effect). Aluminium-based ones can lead to constipation, while those with magnesium can open the floodgates on the other end. If you have kidney disease or are pregnant, check labels and talk to your doctor before picking a product.
H2 blockers generally have fewer dramatic downsides than PPIs when used short-term, but regular use can mean headaches or dizziness. Pepcid (famotidine), for example, is well tolerated, but some people notice odd dreams or confusion, especially in older adults. Watch out if you take other meds: cimetidine (Tagamet) can mess with how your body handles a bunch of common prescriptions, from blood thinners to antidepressants.
On the PPI front, extended use above OTC courses can lead to bigger problems: your risk of things like low magnesium, B12 deficiency, intestinal infections (like C. diff), and possibly bone fractures goes up. Doctors often call it “PPI creep” when folks stay on them for months or years, because nobody got around to reviewing their repeated purchases. If you need a maintenance plan longer than two weeks, your GP should figure out why the reflux is sticking around.
For the anxious types: there’s little evidence that occasional or short-term OTC PPI use causes cancer or dementia. This gets tons of headlines, but the actual science says those links are weak and only a possible risk with heavy, indefinite use. Still, if you’re hitting the PPI pack every month, that’s your cue to ask a doctor to check for H. pylori, hernias, or even rare trouble like Barrett’s Esophagus.
One tip: always read labels for possible allergens—lactose, gluten, and dyes pop up in a surprising number of heartburn meds, and a bad reaction isn’t worth the risk. If you’re grabbing something for a kid, or you’re pregnant or breastfeeding, stick to tried-and-true options—antacids most often, low-dose H2 blockers for older teens and adults—after talking to your doctor.
And watch the clock: if you’re stacking meds with every meal and still burping flames, or wake up most nights with burning, never just keep layering OTC fixes. New chest pain, trouble swallowing, vomiting blood, or dark stools are all medical red flags. That’s when you stop experimenting and see a pro, stat.
For anyone who wants a deeper dive on therapy comparisons, check out this handy post that lays out the key differences between the top choices for a substitute for Nexium 40 mg.

Practical Tips and Lifestyle Tweaks That Boost the Effectiveness of OTC Heartburn Relief
Medicine isn’t the only line of defense against heartburn. Tiny daily tweaks can cut symptoms as much as doubling up on pills—not exaggerating! Start by spacing meals so your stomach isn’t always full; two to three hours between dinner and bed can do wonders. Prop up your head at night using a pillow wedge—gravity is your friend here, literally. Ditching super-tight clothes (yeah, even those trendy jeans) relieves pressure on your stomach, so acid is less likely to want a return trip up your esophagus.
Cutting back on triggers is probably the oldest heartburn advice, but it’s still legit. Coffee, citrus, spicy food, chocolate—these are the big offenders, but some people are sensitive to onions, tomato sauce, or even fizzy drinks. If you’re not sure, keep a quick food diary and scan for a pattern. Those moments reveal a ton, and often a simple change prevents you needing to take more (or stronger) meds.
Smoking is a massive heartburn driver. Nicotine weakens your lower esophageal sphincter, basically letting acid cruise upward without a fight. Fast fact: smokers are twice as likely to have regular reflux compared to non-smokers. Quitting improves symptoms even before you see bigger health benefits. On a related note, cutting back on booze—especially red wine, beer, and spirits—matters. These relax that crucial valve as well.
Weight loss comes up a lot with heartburn for a reason: even trimming five kilos can ease stomach pressure and blunt reflux after meals. If you carry extra weight around your middle, it’s especially key. One Melbourne study showed people who lost just 10% of their body weight cut their need for daily acid meds by half after three months.
Last pro tip: chewing gum after meals (preferably sugar-free) actually triggers more saliva, which helps neutralize acid that sneaks into your esophagus. Sounds ridiculous, but it works. Just skip anything minty—peppermint can make reflux worse for some people.
If you still find yourself returning to the pharmacy aisle, debate whether your heartburn is severe and persistent, comes with other symptoms like unexplained weight loss or blood, or just won’t budge after trying these steps and a decent course of OTC therapy. That’s exactly when to bring in a GP, even before considering a repeat script for Nexium 40 mg. And if your symptoms ease off with a new OTC routine, it’s worth checking every few months to see if you still need medicine at all. Most heartburn can actually be managed down to the bare minimum, saving both money and hassle.



In the grand theater of gastrointestinal chemistry, the balance of gastric acid is nothing short of a metaphysical duel between fire and restraint.
One must appreciate that the body, in its infinite wisdom, does not dispense acid indiscriminately but rather calibrates secretion with culinary demand.
Yet we, the modern denizen of pharmacy aisles, have reduced this elegant equilibrium to a commodity measured in milligrams.
When you reach for an over‑the‑counter proton pump inhibitor, you are, in effect, borrowing the script of a physician without the requisite dialogue.
The danger lies not in the pill per se, but in the hubris of assuming that a 20 mg capsule can faithfully emulate a 40 mg prescription.
Remember, the pharmacodynamics of PPIs require a cascade of enzymatic events that cannot be rushed by doubling doses.
Thus, prudent stewardship of these agents is as much an act of humility as it is of self‑care.