Myasthenia Gravis Antibiotic Safety Checker
Check Antibiotic Safety for MG
Enter an antibiotic name to see its risk level for myasthenia gravis patients based on the latest Cleveland Clinic study data.
When you have myasthenia gravis (MG), even a simple infection can turn dangerous. That’s because the same antibiotics meant to treat that infection might also make your muscle weakness worse. It’s a tightrope walk: treat the infection, or risk triggering a myasthenic crisis. And this isn’t theoretical - it happens. About 2% of MG patients experience a worsening of symptoms after taking certain antibiotics, according to a 2024 study from the Cleveland Clinic involving over 900 antibiotic courses in 365 patients. For some, that means trouble breathing, swallowing, or even needing emergency care.
How Antibiotics Can Worsen Myasthenia Gravis
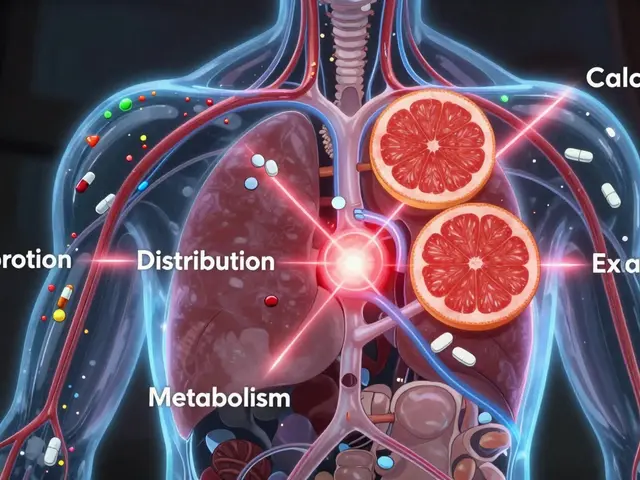
Myasthenia gravis attacks the connection between nerves and muscles. Normally, nerves release acetylcholine, a chemical that tells muscles to contract. In MG, your immune system destroys many of the receptor sites that grab onto acetylcholine. So your muscles don’t get the signal - and they don’t move well.
Some antibiotics interfere with this process, too. They don’t target your immune system, but they mess with the neuromuscular junction in one of three ways:
- They block calcium channels, so nerves can’t release acetylcholine properly.
- They bind to the remaining acetylcholine receptors, stopping the chemical from working.
- They do both.
For someone with MG, this is like removing the last few working lightbulbs in a dim room. The result? Sudden, severe weakness - sometimes in the muscles that control breathing. That’s called a myasthenic crisis. It’s life-threatening and often requires ICU care.
Which Antibiotics Are Riskiest?
Not all antibiotics are created equal when it comes to MG. Some are safe. Others are dangerous. And some fall somewhere in between.
High-risk antibiotics:
- Aminoglycosides - gentamicin, tobramycin, neomycin. These are the worst offenders. They directly block acetylcholine receptors. Avoid them unless there’s absolutely no other option - like a life-threatening infection with no alternatives.
- Fluoroquinolones - ciprofloxacin, levofloxacin, moxifloxacin. These used to be black-box warnings from the FDA for MG patients. They carry a 2.4% risk of triggering worsening symptoms with ciprofloxacin, and 1.9% overall. Still, recent data shows the risk isn’t as high as once thought - but caution is still needed.
- Macrolides - azithromycin, clarithromycin, erythromycin. These have a 1.5% risk of worsening MG. The FDA doesn’t have a black-box warning for these anymore, but case reports still show problems.
- Telithromycin - This drug was pulled from the U.S. market in 2007 because of severe liver damage and MG exacerbations. It’s still a cautionary tale. If you hear it mentioned, know it’s banned for good reason.
Lower-risk antibiotics:
- Penicillins - amoxicillin, ampicillin, penicillin V. These are the go-to choices for most MG patients. The Cleveland Clinic study found only a 1.3% exacerbation rate - the lowest of any class studied. They’re generally safe, even for people with unstable MG.
- Cephalosporins - cefdinir, cephalexin. These are also considered low-risk, though data is more limited than for penicillins.
- Clindamycin - Use with care. It’s not as risky as aminoglycosides, but it’s been linked to MG flares in some cases.
Intermediate-risk antibiotics:
- Tetracyclines - doxycycline, minocycline. These are usually okay for mild infections, but monitor closely.
- Trimethoprim-sulfamethoxazole - Bactrim. Can be used, but watch for fatigue or breathing changes.
- Linezolid - Used for resistant infections. Risk is unclear, but case reports suggest caution.
Who’s at Highest Risk for an Antibiotic-Induced Crisis?
Not every MG patient reacts the same way. Some people can take a fluoroquinolone with no issues. Others crash after one dose. Why? Three key factors make you more vulnerable:
- Recent hospitalization or ER visit - If you’ve been hospitalized or gone to the ER for MG in the last six months, your system is already fragile. Your risk jumps significantly.
- Female sex - Women with MG are more likely to have an antibiotic-triggered flare. The reason isn’t fully understood, but hormones and immune differences may play a role.
- Diabetes - This condition seems to make the neuromuscular junction more sensitive to drug interference. If you have diabetes and MG, you’re in a higher-risk group.
Age and kidney function matter too. Older patients and those with reduced kidney function clear drugs slower. That means antibiotics stick around longer - increasing the chance of buildup and toxicity.

What If You Need a High-Risk Antibiotic?
Here’s the hard truth: sometimes, you have to use a risky antibiotic. A lung infection, a urinary tract infection that won’t quit, or a skin infection spreading fast - these can kill you faster than an MG flare.
So what do you do?
- Don’t delay treatment. Infection is the #1 trigger of MG flares - not antibiotics. In fact, 88.2% of the flare-ups linked to antibiotics in the Cleveland study were actually caused by the infection itself. Treating the infection often helps the MG more than the drug hurts it.
- Choose the safest option possible. Can you use amoxicillin instead of ciprofloxacin? Use cephalexin instead of azithromycin? Always ask.
- Get a specialist’s input. Talk to your neurologist or MG specialist before starting any new antibiotic. Don’t rely on your primary care doctor alone.
- Monitor closely. If you’re on a higher-risk drug, check in daily for the first 72 hours. Are you having more trouble swallowing? Is your vision blurrier? Are you short of breath? Call your doctor immediately if you notice any change.
- Have a rescue plan. Know where your nearest emergency center is. Keep your emergency MG medication (like pyridostigmine) on hand. Tell someone close to you what signs to watch for.
What Should You Do Before Taking Any Antibiotic?
There’s no magic checklist, but these steps can save your life:
- Always tell every doctor and pharmacist you have MG. Even if it’s your dentist or a walk-in clinic. Put it in your medical alert bracelet or phone wallet.
- Keep a list of safe and unsafe antibiotics. Update it yearly. The Myasthenia Gravis Foundation of America has a public list that’s updated quarterly.
- Don’t take leftover antibiotics. Even if they’re “safe” ones like amoxicillin - if they’re old, they might not work. And if they’re risky ones like ciprofloxacin, don’t risk it.
- Ask: Is this antibiotic really necessary? Many infections - especially viral ones - don’t need antibiotics. Don’t pressure your doctor for a script.
- Use one pharmacy. That way, your pharmacist can flag dangerous interactions. They’re often the last line of defense.

Why the Guidelines Are Changing
For years, doctors were told: avoid fluoroquinolones and macrolides in MG patients. Full stop. But the 2024 Cleveland Clinic study changed that. It wasn’t just another case report. It was the largest, most detailed study ever done on this topic - 365 patients, over 900 antibiotic courses, tracked over 20 years.
The results? The risk of a flare from fluoroquinolones and macrolides was only slightly higher than from penicillins - and not statistically significant. That means, for many stable MG patients, these drugs might be okay with proper monitoring.
This isn’t a green light to use them freely. But it’s a shift from fear-based avoidance to smart, risk-stratified use. Neurologists are now starting to say: “We don’t need to avoid these drugs - we need to watch for warning signs.”
Final Thought: It’s About Balance
Myasthenia gravis is already a battle. You shouldn’t have to fear every antibiotic. But you also shouldn’t ignore the risks. The goal isn’t to avoid all antibiotics - it’s to choose the right one, at the right time, with the right support.
When infection strikes, your body is fighting two wars: one against the bug, and one against your own immune system. The right antibiotic can tip the scales in your favor. The wrong one? It can turn a bad day into a crisis.
Stay informed. Stay connected to your care team. And never assume an antibiotic is safe just because it’s common. Your muscles are counting on you to ask the right questions.
Can I take amoxicillin if I have myasthenia gravis?
Yes, amoxicillin is one of the safest antibiotics for people with myasthenia gravis. Studies show only a 1.3% risk of triggering a flare - the lowest among all antibiotic classes. It’s commonly recommended by MG specialists and is often the first choice for infections like sinusitis, strep throat, or urinary tract infections. Still, always tell your doctor you have MG before starting any medication.
Are fluoroquinolones completely banned for MG patients?
No, they’re not banned, but they’re strongly discouraged. The FDA issued black box warnings for fluoroquinolones like ciprofloxacin and levofloxacin due to their link to MG worsening. However, newer research shows the actual risk is low - around 2% - and similar to safer antibiotics like amoxicillin. For stable MG patients with no recent hospitalizations, these drugs may be used cautiously if no alternatives exist. Always monitor closely for signs of increased weakness.
What should I do if I start feeling weaker after taking an antibiotic?
Stop the antibiotic and contact your neurologist or MG specialist immediately. If you’re having trouble breathing, swallowing, or speaking, go to the emergency room. These could be signs of a myasthenic crisis. Don’t wait. Bring the antibiotic bottle with you. Many MG patients recover quickly once the drug is stopped, but delays can be life-threatening.
Can infections themselves trigger MG flares without antibiotics?
Yes - and they’re the most common trigger. In fact, 88.2% of MG flares that happen after antibiotic use are actually caused by the infection, not the drug. That’s why treating infections promptly is critical. Sometimes, the antibiotic is helping more than it’s hurting. The key is choosing the safest option available and watching for worsening symptoms.
Should I avoid all antibiotics if I have MG?
No. Avoiding antibiotics entirely is dangerous. Untreated infections can lead to pneumonia, sepsis, or respiratory failure - all far more deadly than a drug-induced MG flare. The goal isn’t to avoid antibiotics, but to use them wisely. Work with your care team to pick the safest drug for your infection, and always monitor for changes in strength or breathing.
Is there a list of safe antibiotics I can keep on hand?
Yes. The Myasthenia Gravis Foundation of America maintains a publicly updated list of cautionary and safe drugs. Safe options include penicillins (amoxicillin, ampicillin), cephalosporins (cephalexin), and some macrolides in stable patients. High-risk drugs include aminoglycosides (gentamicin), fluoroquinolones (ciprofloxacin), and telithromycin. Print this list and keep it in your wallet or phone. Share it with every provider who prescribes you medication.



Amoxicillin is your best friend if you’ve got MG. I’ve been on it three times in the last year for sinus infections and zero issues. Just tell every doc you see - even the dentist - and you’ll be fine.